It is estimated that more than one-third of patients treated for skin disorders have underlying psychiatric problems complicating their skin conditions.[RD1] The skin is a vital organ of communication and its role begins in early development and remains important throughout our life. Welcome to the study of psychodermatology which treats the connection between psychiatry and dermatology.
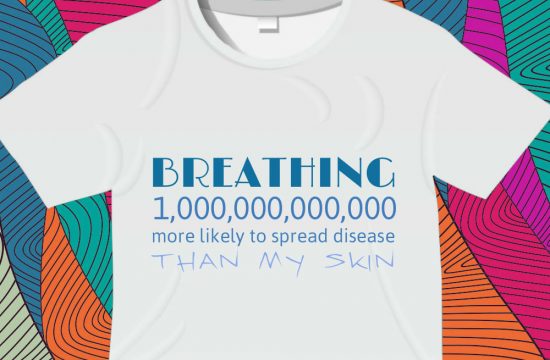
Stress is one of the major and most important factors that starts and continually triggers skin diseases. Psoriasis is considered to be a psychophysiologic condition, one of the conditions of psychodermatology. This is because the skin problem is not directly connected to the mind but reacts to emotional states such as stress.
The first recorded case of psychodermatosis dates back to 1700 B.C., when the physicians to the prince of Persia conceded that the prince’s psoriasis was caused by anxiety over succeeding his father to the throne.1[RD2]
In modern and traditional medicine beliefs, the skin is known as the organ which is responsible for feelings such as touch, temperature and pain, almost like an emotional gateway to our external environment. Therefore, skin has an important role to play in our physical and mental wellness. People with a skin disorder almost always experience physical, mental and socioeconomic embarrassment in their society. This embarrassment leads to mental stress which further causes aggravation of the skin disease.
Since that time in 1700BC in Persia, physicians have become aware of how much emotional states impact on skin diseases and how the skin can reflect a person’s psychological state.
Depression, anxiety, and anger are the most commonly observed emotional reactions in individuals with skin disease. There is clear evidence that negative emotional states such as stress, anxiety, depression, and anger can also exacerbate skin disease.
Several techniques are recommended in psychiatry that may improve skin disorders, reduce psychological distress, and increase the quality of life of the affected individual.
Biofeedback
Biofeedback is a non-invasive conditioning technique with wide applications in the field of medicine. Biofeedback can enhance the patient’s awareness of tension and help them to relax, thus help in improving skin disorders that flare with stress or that has an autonomic nervous system aspect. Electromyography (EMG, muscle tension) and blood flow (temperature) training are the most commonly used modalities. Patients are taught relaxation techniques and their effects can be directly observed by the patients in terms of changes in muscle tension, blood flow, heart rate, or other parameters paralleling desired improvements. Biofeedback can help reduce the stress that tends to exacerbate many inflammatory skin disorders.
Cognitive behavioural therapy
Cognitive–behavioural therapy (CBT) is a treatment that changes harmful or destructive ways of thinking, feeling and behaving through the use of cognitive and behavioural interventions. CBT therapy alters dysfunctional habits by interrupting changing thought patterns (cognitions) or actions (behaviors) that cause disease in the skin.
Hypnosis
Hypnotic techniques and the trance state have been used since ancient times to assist in healing. There are many myths about hypnosis, however, the main purpose of medical hypnotherapy is to reduce suffering and promote healing. Hypnosis may improve or clear many skin disorders. Hypnosis alters the neurohormonal systems that in turn regulate many body functions and facilitate the mind-body connection to promote healing.
NICS
Psychodermatology looks at the interaction between mind and skin. Psychiatry is more focused on the internal, non visible disease, and dermatology is focused on the external visible disease. Connecting the two disciplines is an interplay between neuroendocrine and immune systems that has been described as the neuro-immuno-cutaneous system (NICS). The NICS is an interaction between the nervous system, skin, and immunity. This ultimately, is the link that completes the mind, body and soul approach to treating psoriasis.
Holisitic regards
Satyapal Singh, J.S. Tripathi, N.P. Rai, S, 2014. An overview of Ayurvedic & contemporary approaches to Psychodermatology. The Journal of Phytopharmacology, 3(4), 286-299.
http://www.phytopharmajournal.com/Vol3_Issue4_10.pdf
1. Shafii, M& Shafii, S. Exploratory psychotherapy in the treatment of psoriasis. Twelve hundred years ago. Archives of general psychiatry1979; 36(11):1242-1245.